
Parkinson’s Disease
•
• Parkinson’s disease facts
• What is Parkinson’s disease?
• What causes Parkinson’s disease?
• What genes are linked to Parkinson’s disease?
• Who is at risk for Parkinson’s disease?
• What are the symptoms of Parkinson’s disease?
• What other conditions resemble Parkinson’s disease?
• How is Parkinson’s disease diagnosed?
• What is the treatment for Parkinson’s disease?
• How can people learn to cope with Parkinson’s disease?
• Can Parkinson’s disease be prevented?
• What is the prognosis of Parkinson’s disease?
•
Take the Parkinson’s Quiz
• Parkinson’s Disease Center
• Parkinson’s Disease Slideshow Pictures
• Dementia Slideshow Pictures
• Take the Parkinson’s Quiz
• Parkinson’s Disease FAQs
• Patient Comments: Parkinson’s Disease – Symptoms
• Patient Comments: Parkinson’s Disease – Treatments
• Patient Comments: Parkinson’s Disease – Diagnosis
• Patient Comments: Parkinson’s Disease – Prognosis
• Find a local Neurologist in your town
• Parkinson’s disease facts
• What is Parkinson’s disease?
• What causes Parkinson’s disease?
• What genes are linked to Parkinson’s disease?
• Who is at risk for Parkinson’s disease?
• What are the symptoms of Parkinson’s disease?
• What other conditions resemble Parkinson’s disease?
• How is Parkinson’s disease diagnosed?
• What is the treatment for Parkinson’s disease?
• How can people learn to cope with Parkinson’s disease?
• Can Parkinson’s disease be prevented?
• What is the prognosis of Parkinson’s disease?
Parkinson’s disease facts
• Parkinson’s disease is a neurodegenerative disorder which leads to progressive deterioration of motor function due to loss of dopamine-producing brain cells.
• Primary symptoms include
o tremor,
o stiffness,
o slowness,
o impaired balance,
o and later on a shuffling gait.
• Some secondary symptoms include
o anxiety,
o depression, and
o dementia.
• Most individuals with Parkinson’s disease are diagnosed when they are 60 years old or older, but early-onset Parkinson’s disease also occurs.
• With proper treatment, most individuals with Parkinson’s disease can lead long, productive lives for many years after diagnosis.
What is Parkinson’s disease?
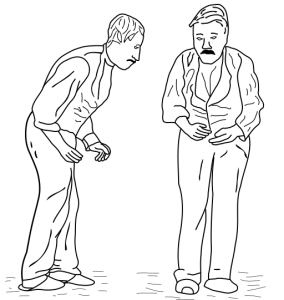
Parkinson’s disease is the second most common neurodegenerative disorder and the most common movement disorder. It is characterized by progressive loss of muscle control, which leads to trembling of the limbs and head while at rest, stiffness, slowness, and impaired balance. As symptoms worsen, it may become difficult to walk, talk, and complete simple tasks.
The progression of Parkinson’s disease and the degree of impairment vary from individual to individual. Many people with Parkinson’s disease live long productive lives, whereas others become disabled much more quickly. Premature death is usually due to complications such as falling-related injuries or pneumonia.
Most individuals who develop Parkinson’s disease are 60 years of age or older. Since overall life expectancy is rising, the number of individuals with Parkinson’s disease will increase in the future. Adult-onset Parkinson’s disease is most common, but early-onset Parkinson’s disease (onset between 21-40 years), and juvenile-onset Parkinson’s disease (onset before age 21) also exist.
Descriptions of Parkinson’s disease date back as far as 5000 BC. Around that time, an ancient Indian civilization called the disorder Kampavata and treated it with the seeds of a plant containing therapeutic levels of what is today known as levodopa. Parkinson’s disease was named after the British doctor James Parkinson, who in 1817 first described the disorder in great detail as “shaking palsy.”
What causes Parkinson’s disease?
A substance called dopamine acts as a messenger between two brain areas – the substantia nigra and the corpus striatum – to produce smooth, controlled movements. Most of the movement-related symptoms of Parkinson’s disease are caused by a lack of dopamine due to the loss of dopamine-producing cells in the substantia nigra. When the amount of dopamine is too low, communication between the substantia nigra and corpus striatum becomes ineffective, and movement becomes impaired; the greater the loss of dopamine, the worse the movement-related symptoms. Other cells in the brain also degenerate to some degree and may contribute to non-movement related symptoms of Parkinson’s disease.
Although it is well known that lack of dopamine causes the motor symptoms of Parkinson’s disease, it is not clear why the dopamine-producing brain cells deteriorate. Genetic and pathological studies have revealed that various dysfunctional cellular processes, inflammation, and stress can all contribute to cell damage. In addition, abnormal clumps called Lewy bodies, which contain the protein alpha-synuclein, are found in many brain cells of individuals with Parkinson’s disease. The function of these clumps in regards to Parkinson’s disease is not understood. In general, scientists suspect that dopamine loss is due to a combination of genetic and environmental factors.
What genes are linked to Parkinson’s disease?
In most individuals, Parkinson’s disease is idiopathic, which means that it arises sporadically with no known cause. However, some of individuals diagnosed with Parkinsons also have family members with the disease. By studying families with hereditary Parkinson’s disease, scientists have identified several genes that are associated with the disorder. Studying these genes helps understand the cause of Parkinson’s disease and may lead to new therapies. So far, five genes have been identified that are definitively associated with Parkinson’s disease.
1. SNCA (synuclein, alpha non A4 component of amyloid precursor): SNCA makes the protein alpha-synuclein. In brain cells of individuals with Parkinson’s disease, this protein aggregates in clumps called Lewy bodies. Mutations in the SNCA gene are found in early-onset Parkinson’s disease.
2. PARK2 (Parkinson’s disease autosomal recessive, juvenile 2): The PARK2 gene makes the protein parkin. Mutations of the PARK2 gene are mostly found in individuals with juvenile Parkinson’s disease. Parkin normally helps cells break down and recycle proteins.
3. PARK7 (Parkinson’s disease autosomal recessive, early onset 7): PARK7 mutations are found in early-onset Parkinson’s disease. The PARK7 gene makes the DJ-1 protein, which may protect cells from oxidative stress.
4. PINK1 (PTEN-induced putative kinase 1): Mutations of this gene are found in early-onset Parkinson’s disease. The exact function of the protein made by PINK1 is not known, but it may protect structures within the cell called mitochondria from stress.
5. LRRK2 (leucine-rich repeat kinase 2): LRRK2 makes the protein dardarin. Mutations in the LRRK2 gene have been linked to late-onset Parkinson’s disease.
Several other chromosome regions and the genes GBA (glucosidase beta acid), SNCAIP (synuclein alpha interacting protein), and UCHL1 (ubiquitin carboxyl-terminal esterase L1) may also be linked to Parkinson’s disease.
Who is at risk for Parkinson’s disease?
• Age is the largest risk factor for the development and progression of Parkinson’s disease. Most people who develop Parkinson’s disease are older than 60 years years of age.
• Men are affected about 1.5 to 2 times more often than women.
• A small number of individuals are at increased risk because of a family history of the disorder.
• Head trauma, illness, or exposure to environmental toxins such as pesticides and herbicides may be a risk factor.
Parkinson’s disease mentioned in history
Descriptions of people with Parkinsonism date back to ancient Egypt. It is also mentioned in the Christian Bible and Claudius Galenus’ (Galen’s) writings. Claudius Galenus (or Aelius Galenus), who lived from 129 AD to around 200 AD, was a well-known Roman (of Greek origin) doctor and philosopher.
Then there seem to be no clear references to PD (Parkinson’s Disease) until the 17th century. Auguste François Chomel, a French pathologist, John Hunter, a Scottish surgeon, Hieronymus David Gaubius, a German physician and chemist, and Franciscus Sylvius, a Dutch chemist, physiologist and anatomist, all described Parkinson’s-type signs and symptoms during the 17th and 18th centuries.
James Parkinson
James Parkinson (1755-1824) – an English apothecary surgeon, political activist, paleontologist and geologist, wrote An Essay on the Shaking Palsy in 1817. In that work he is thought to be the first to describe paralysis agitans (shaking palsy), a condition which Jean-Martin Charcot renamed Parkinson’s disease sixty years later.
James Parkinson systematically described six people with signs and symptoms of the disease we know today as Parkinson’s. They were not formally examined, but he observed them as they went on on their daily walks, and sometimes asked them to describe their symptoms to him. In his Essay Parkinson described the characteristic resting tremor, diminished muscle strength, paralysis, unusual posture and gait, and how the disease progresses over time.
Jean-Martin Charcot (1825-1893) – a French neurologist and professor of anatomical pathology, also known as the founder of modern neurology. His studies between 1868 and 1881 are described today by medical historians as a “landmark in the understanding of Parkinson’s disease”. He also clearly defined and explained the difference between rigidity, weakness and bradykinesia (a slowness in the execution of movement). Charcot is also famous for naming and being the first to describe multiple sclerosis.
Drawing of a patient with Parkinson’s by Charcot
Frederic Lewy (1885-1950) – a prominent American neurologist is best known for the discovery of Lewy bodies, characteristic indicators of Dementia with Lewy Bodies and Parkinson’s disease.
Konstantin Nikolaevitch Tretiakoff (1892-1958) – a Russian neuropathologist. While writing his thesis for his doctorate at L’Assistance Publique des Hopitaux de Paris, France, he described the degeneration of the substantia nigra in cases of Parkinson’s – he was the first to link this anatomic structure with Parkinson’s disease. Tretiakoff’s findings were not accepted by many in the medical community, until they were confirmed in further studies carried out by Rolf Hassler, in 1938.
Rolf Hassler (1914-1984) – a distinguished German pathologist. Hassler made important discoveries in the treatment of Parkinson’s disease. In a 1938 published paper, he wrote that autopsies of Parkinson’s patients showed that the most affected part of the brain was the substantia nigra pars pallidus, which lost many neurons and had an abundant accumulation of Lewy bodies. He became a pioneer in surgery for tremor.
Arvid Carlsson (1923) – a Swedish scientist who was awarded the Nobel Prize in Physiology/Medicine in 2000 for his work on dopamine, Carlsson is best known for his work with dopamine and its effects in Parkinson’s disease. He demonstrated that dopamine is a neurotransmitter in the brain and not just a precursor for norepinephrine.
Carlsson and his research team at Astra AB (today AstraZeneca) managed to derive the first marketed SSRI (selective serotonin reuptake inhibitor) – zimelidine – from brompheniramine. He noticed that dopamine levels in the basal ganglia are particularly high – this part of the brain is important for movement. He then demonstrated that when animals were given reserpine, a drug, dopamine levels dropped and the animals lost movement control – he explained that in Parkinson’s disease, dopamine levels also fall, causing loss of movement.
Carlsson then showed that when L-Dopa was administered to the animals, their symptoms were alleviated. L-Dopa is a precursor of dopamine. This breakthrough led doctors to try L-Dopa on their Parkinson’s patients with early symptoms. L-Dopa is still the basis for most drugs prescribed for Parkinson’s disease symptoms.
Kazimierz Funk (anglicized as Casimir Funk 1884 – 1967) – a Polish biochemist. Until the arrival of “levodopa”, anticholinergics and surgery were the only available treatments for patients with Parkinson’s. Funk first synthesized levodopa (L-Dopa) in 1911, but it was not until the middle of the last century that it received any attention. In 1967, levodopa entered clinical practice and revolutionized Parkinson’s management.
Well known people with Parkinson’s disease
Alive (as at 26th June, 2012)
• Billy Graham (b. 1918), American evangelist
• Booth Gardner (b. 1936), Washington state governor
• Gunther von Hagens (b. 1945), Inventor and Anatomist
• Janet Reno (b. 1938), Former Attorney General of the United States
• Jansher Khan (b. 1969), ex-World squash champion
• Jeremy Thorpe (b. 1929), British politician
• John Walker (b. 1952), New Zealand athlete
• Maurice White (b. 1941), musician
• Michael J. Fox (b. 1961), Canadian actor
• Muhammad Ali (b. 1942), boxer (pugilistic Parkinson’s syndrome)
• Ray Kennedy (b. 1951), English soccer player
Dead
• Basil D’Oliveira (1931-2011), South African born English cricketer
• Charles Schulz, American cartoonist (1922-2000)
• Deborah Kerr, British actress (1921-2007)
• Enoch Powell, British politician (1912-1998)
• Eugene McCarthy (1916-2005) American politician
• Francisco Franco Spanish dictator (1892-1975)
• George Wallace, former governor of Alabama (1919-1998)
• John Lindsay, New York City mayor (1921-2000)
• Kenneth More, English actor (1914-1982)
• Mao Zedong, Chinese Dictator (1893-1976)
• Pierre Elliott Trudeau, Canadian politician (1919-2000)
• Pope John Paul II (1920-2005), Polish cleric
• Prince Claus, (1926-2002), husband of Queen Beatrix of the Netherlands
• Salvador Dalí, Spanish artist (1904-1989)
• Sir John Betjeman, CBE, British Poet Laureate (1906-1984)
• Sir Michael Redgrave (1908-1985), British actor
• Terry-Thomas, British character actor (1911-1990)
• Vincent Price, American actor, also suffered from lung cancer (1911-1993)
