Carpal tunnel syndrome (CTS) is an entrapment median neuropathy, causing paresthesia, pain, numbness, and other symptoms in the distribution of the median nerve due to its compression at the wrist in the carpal tunnel. The pathophysiology is not completely understood but can be considered compression of the median nerve traveling through the carpal tunnel.[1] The National Center for Biotechnology Information and highly cited literature[2] say the most common cause of CTS is typing.[3] Research by Lozano-Calderón has cited genetics as a factor,[4] and has encouraged caution in ascribing causality.[5]
The main symptom of CTS is intermittent numbness of the thumb, index, long and radial half of the ring finger.[6] The numbness often occurs at night, with the hypothesis that the wrists are held flexed during sleep. Recent literature suggests that sleep positioning, such as sleeping on one’s side, might be an associated factor.[7] It can be relieved by wearing a wrist splint that prevents flexion.[8] Long-standing CTS leads to permanent nerve damage with constant numbness, atrophy of some of the muscles of the thenar eminence, and weakness of palmar abduction.[9]
Pain in carpal tunnel syndrome is primarily numbness that is so intense that it wakes one from sleep. Pain in electrophysiologically verified CTS is associated with misinterpretation of nociception and depression.[10]
Palliative treatments for CTS include use of night splints and corticosteroid injection. The only scientifically established disease modifying treatment is surgery to cut the transverse carpal ligament.[11]
Signs and symptoms
Patients with CTS experience numbness, tingling, or burning sensations in the thumb and fingers, in particular the index, middle fingers, and radial half of the ring fingers, which are innervated by the median nerve. Less-specific symptoms may include pain in the wrists or hands and loss of grip strength[12] (both of which are more characteristic of painful conditions such as arthritis).
Some posit that median nerve symptoms can arise from compression at the level of the thoracic outlet or the area where the median nerve passes between the two heads of the pronator teres in the forearm,[13] but this is highly debatable. This line of thinking is an attempt to explain pain and other symptoms not characteristic of carpal tunnel syndrome.[14] Carpal tunnel syndrome is a common diagnosis with an objective, reliable, verifiable pathophysiology, whereas thoracic outlet syndrome and pronator syndrome are defined by a lack of verifiable pathophysiology and are usually applied in the context of nonspecific upper extremity pain.
Numbness and paresthesias in the median nerve distribution are the hallmark neuropathic symptoms (NS) of carpal tunnel entrapment syndrome. Weakness and atrophy of the thenar muscles may occur if the condition remains untreated.[15]
Causes
Most cases of CTS are of unknown causes, or idiopathic.[16] Carpal Tunnel Syndrome can be associated with any condition that causes pressure on the median nerve at the wrist. Some common conditions that can lead to CTS include obesity, oral contraceptives, hypothyroidism, arthritis, diabetes, and trauma.[17] Carpal tunnel is also a feature of a form of Charcot-Marie-Tooth syndrome type 1 called hereditary neuropathy with liability to pressure palsies.
Other causes of this condition include intrinsic factors that exert pressure within the tunnel, and extrinsic factors (pressure exerted from outside the tunnel), which include benign tumors such as lipomas, ganglion, and vascular malformation.[18] Carpal tunnel syndrome often is a symptom of transthyretin amyloidosis-associated polyneuropathy and prior carpal tunnel syndrome surgery is very common in individuals who later present with transthyretin amyloid-associated cardiomyopathy, suggesting that transthyretin amyloid deposition may cause carpal tunnel syndrome.[19][20][21][22][23][24][25]
Work related
The international debate regarding the relationship between CTS and repetitive motion in work is ongoing. The Occupational Safety and Health Administration (OSHA) has adopted rules and regulations regarding cumulative trauma disorders. Occupational risk factors of repetitive tasks, force, posture, and vibration have been cited. However, the American Society for Surgery of the Hand (ASSH) has issued a statement claiming that the current literature does not support a causal relationship between specific work activities and the development of diseases such as CTS.[26]
The relationship between work and CTS is controversial; in many locations, workers diagnosed with carpal tunnel syndrome are entitled to time off and compensation.[27] In the USA, carpal tunnel syndrome results in an average of $30,000 in lifetime costs (medical bills and lost time from work).[28]
Some speculate that carpal tunnel syndrome is provoked by repetitive movement and manipulating activities and that the exposure can be cumulative. It has also been stated that symptoms are commonly exacerbated by forceful and repetitive use of the hand and wrists in industrial occupations,[29] but it is unclear as to whether this refers to pain (which may not be due to carpal tunnel syndrome) or the more typical numbness symptoms.[30]
A review of available scientific data by the National Institute for Occupational Safety and Health (NIOSH) indicated that job tasks that involve highly repetitive manual acts or specific wrist postures were associated with incidents of CTS, but causation was not established, and the distinction from work-related arm pains that are not carpal tunnel syndrome was not clear. It has been proposed that repetitive use of the arm can affect the biomechanics of the upper limb or cause damage to tissues. It has also been proposed that postural and spinal assessment along with ergonomic assessments should be included in the overall determination of the condition. Addressing these factors has been found to improve comfort in some studies.[31]
Speculation that CTS is work-related is based on claims such as CTS being found mostly in the working adult population, though evidence is lacking for this. For instance, in one recent representative series of a consecutive experience, most patients were older and not working.[32] Based on the claimed increased incidence in the workplace, arm use is implicated, but the weight of evidence suggests that this is an inherent, genetic, slowly but inevitably progressive idiopathic peripheral mononeuropathy.[33]
Associated with other diseases
A variety of patient factors can lead to CTS, including heredity, size of the carpal tunnel, associated local and systematic diseases, and certain habits.[1] Non-traumatic causes generally happen over a period of time, and are not triggered by one certain event. Many of these factors are manifestations of physiologic aging.[34]
Examples include:
- Rheumatoid arthritis and other diseases that cause inflammation of the flexor tendons.
- With hypothyroidism, generalized myxedema causes deposition of mucopolysaccharides within both the perineurium of the median nerve, as well as the tendons passing through the carpal tunnel.
- During pregnancy women experience CTS due to hormonal changes (high progesterone levels) and water retention (which swells the synovium), which are common during pregnancy.
- Previous injuries including fractures of the wrist.
- Medical disorders that lead to fluid retention or are associated with inflammation such as: inflammatory arthritis, Colles’ fracture, amyloidosis, hypothyroidism, diabetes mellitus, acromegaly, and use of corticosteroids and estrogens.
- Carpal tunnel syndrome is also associated with repetitive activities of the hand and wrist, in particular with a combination of forceful and repetitive activities[17]
- Acromegaly causes excessive growth hormones. This causes the soft tissues and bones around the carpel tunnel to grow and compress the median nerve.[35]
- Tumors (usually benign), such as a ganglion or a lipoma, can protrude into the carpal tunnel, reducing the amount of space. This is exceedingly rare (less than 1%).
- Obesity also increases the risk of CTS: individuals classified as obese (BMI > 29) are 2.5 times more likely than slender individuals (BMI < 20) to be diagnosed with CTS.[36]
- Double-crush syndrome is a debated hypothesis that compression or irritation of nerve branches contributing to the median nerve in the neck, or anywhere above the wrist, increases sensitivity of the nerve to compression in the wrist. There is little evidence, however, that this syndrome really exists.[37]
- Heterozygous mutations in the gene SH3TC2, associated with Charcot-Marie-Tooth, confer susceptibility to neuropathy, including the carpal tunnel syndrome.[38]
- Parvovirus b19 has been associated with carpel tunnel syndrome [39]
Diagnosis
There is no consensus reference standard for the diagnosis of carpal tunnel syndrome. A combination of described symptoms, clinical findings, and electrophysiological testing is used by a majority of hand surgeons. Numbness in the distribution of the median nerve, nocturnal symptoms, thenar muscle weakness/atrophy, positive Tinel’s sign at the carpal tunnel, and abnormal sensory testing such as two-point discrimination have been standardized as clinical diagnostic criteria by consensus panels of experts.[40][41] A predominance of pain rather than numbness is unlikely to be caused by carpal tunnel syndrome no matter what the result of electrophysiological testing.
Electrodiagnostic testing (electromyography and nerve conduction velocity) can objectively verify the median nerve dysfunction. If these tests are normal, carpal tunnel syndrome is either absent or very, very mild.
Clinical assessment by history taking and physical examination can support a diagnosis of CTS.
- Phalen’s maneuver is performed by flexing the wrist gently as far as possible, then holding this position and awaiting symptoms.[42] A positive test is one that results in numbness in the median nerve distribution when holding the wrist in acute flexion position within 60 seconds. The quicker the numbness starts, the more advanced the condition. Phalen’s sign is defined as pain and/or paresthesias in the median-innervated fingers with one minute of wrist flexion. Only this test has been shown to correlate with CTS severity when studied prospectively.[1]
- Tinel’s sign, a classic — though less sensitive – test is a way to detect irritated nerves. Tinel’s is performed by lightly tapping the skin over the flexor retinaculum to elicit a sensation of tingling or “pins and needles” in the nerve distribution. Tinel’s sign (pain and/or paresthesias of the median-innervated fingers with percussion over the median nerve) is less sensitive, but slightly more specific than Phalen’s sign.[1]
- Durkan test, carpal compression test, or applying firm pressure to the palm over the nerve for up to 30 seconds to elicit symptoms has also been proposed.[43][44]
As a note, a patient with true carpal tunnel syndrome (entrapment of the median nerve within the carpal tunnel) will not have any sensory loss over the thenar eminence (bulge of muscles in the palm of hand and at the base of the thumb). This is because the palmar branch of the median nerve, which innervates that area of the palm, branches off of the median nerve and passes over the carpal tunnel.[45] This feature of the median nerve can help separate carpal tunnel syndrome from thoracic outlet syndrome, or pronator teres syndrome.
Other conditions may also be misdiagnosed as carpal tunnel syndrome. Thus, if history and physical examination suggest CTS, patients will sometimes be tested electrodiagnostically with nerve conduction studies and electromyography. The goal of electrodiagnostic testing is to compare the speed of conduction in the median nerve with conduction in other nerves supplying the hand. When the median nerve is compressed, as in CTS, it will conduct more slowly than normal and more slowly than other nerves. There are many electrodiagnostic tests used to make a diagnosis of CTS, but the most sensitive, specific, and reliable test is the Combined Sensory Index (also known as Robinson index).[46] Electrodiagnosis rests upon demonstrating impaired median nerve conduction across the carpal tunnel in context of normal conduction elsewhere. Compression results in damage to the myelin sheath and manifests as delayed latencies and slowed conduction velocities [1] However, normal electrodiagnostic studies do not preclude the presence of carpal tunnel syndrome, as a threshold of nerve injury must be reached before study results become abnormal and cut-off values for abnormality are variable.[41] Carpal tunnel syndrome with normal electrodiagnostic tests is very, very mild at worst.
The role of MRI or ultrasound imaging in the diagnosis of carpal tunnel syndrome is unclear.[47][48][49]
Differential diagnosis
There are some who believe that carpal tunnel syndrome is simply a universal label applied to anyone suffering from pain, numbness, swelling, and/or burning in the radial side of the hands and/or wrists. When pain is the primary symptom, carpal tunnel syndrome is unlikely to be the source of the symptoms.[30] As a whole, the medical community is not currently embracing or accepting trigger point theories due to lack of scientific evidence supporting their effectiveness.[50]
Pathophysiology
Main article: Carpal tunnel
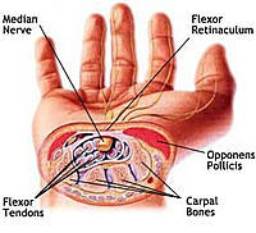
The carpal tunnel is an anatomical compartment located at the base of the palm. Nine flexor tendons and the median nerve pass through the carpal tunnel that is surrounded on three sides by the carpal bones that form an arch. The median nerve provides feeling or sensation to the thumb, index finger, long finger, and half of the ring finger. At the level of the wrist, the median nerve supplies the muscles at the base of the thumb that allow it to abduct, or move away from the fingers, out of the plane of the palm. The carpal tunnel is located at the middle third of the base of the palm, bounded by the bony prominence of the scaphoid tubercle and trapezium at the base of the thumb, and the hamate hook that can be palpated along the axis of the ring finger. The proximal boundary is the distal wrist skin crease, and the distal boundary is approximated by a line known as Kaplan’s cardinal line.[51] This line uses surface landmarks, and is drawn between the apex of the skin fold between the thumb and index finger to the palpated hamate hook.[52] The median nerve can be compressed by a decrease in the size of the canal, an increase in the size of the contents (such as the swelling of lubrication tissue around the flexor tendons), or both.[53] Simply flexing the wrist to 90 degrees will decrease the size of the canal.
Compression of the median nerve as it runs deep to the transverse carpal ligament (TCL) causes atrophy of the thenar eminence, weakness of the flexor pollicis brevis, opponens pollicis, abductor pollicis brevis, as well as sensory loss in the digits supplied by the median nerve. The superficial sensory branch of the median nerve, which provides sensation to the base of the palm, branches proximal to the TCL and travels superficial to it. Thus, this branch spared in carpal tunnel syndrome, and there is no loss of palmar sensation.[54]
Prevention
A systematic review in 2007 of the published English-language literature assessed the quality and strength of articles addressing causes for carpal tunnel syndrome. The authors applied the Bradford Hill criteria to papers on various biological and occupational factors that have been proposed to have a causative effect. Biological factors such as genetic predisposition and anthropometrics had significantly stronger causal association with carpal tunnel syndrome than occupational/environmental factors such as repetitive hand use and stressful manual work.[55] This suggests that carpal tunnel syndrome might not be preventable simply by avoiding certain activities or types of work/activities. Suggested healthy habits such as avoiding repetitive stress, work modification through use of ergonomic equipment (wrist rest, mouse pad), taking proper breaks, using keyboard alternatives (digital pen, voice recognition, and dictation), and employing early treatments such as taking turmeric (anti-inflammatory), omega-3 fatty acids, and B vitamins have been proposed as methods to help prevent carpal tunnel syndrome. The potential role of B-vitamins in preventing or treating carpal tunnel syndrome has not been proven.[56][57] There is little or no data to support the concept that activity adjustment prevents carpal tunnel syndrome.[55]
Treatment
There have been numerous scientific papers evaluating treatment efficacy in CTS. It is important to distinguish treatments that are supported in the scientific literature from those that are advocated by any particular device manufacturer or any other party with a vested financial interest. Generally accepted treatments, as described below, may include splinting or bracing, steroid injection, activity modification, physiotherapy, regular massage therapy treatments,medications, and surgical release of the transverse carpal ligament.
According to the 2007 guidelines by the American Academy of Orthopaedic Surgeons,[58] early surgery with carpal tunnel release is indicated where there is clinical evidence of median nerve denervation or the patient elects to proceed directly to surgical treatment. Otherwise, the main recommended treatments are local corticosteroid injection, splinting (immobilizing braces), oral corticosteroids and ultrasound treatment. The treatment should be switched when the current treatment fails to resolve the symptoms within 2 to 7 weeks. However, these recommendations have sufficient evidence for carpal tunnel syndrome when found in association with the following conditions: diabetes mellitus, coexistent cervical radiculopathy, hypothyroidism, polyneuropathy, pregnancy, rheumatoid arthritis, and carpal tunnel syndrome in the workplace.[58]
In a working population, Lyall demonstrated an earlier return to work and a greater percentage of those able to return to work in patients treated with early carpal tunnel release compared to those who spent time involved in nonoperative treatment, such as injections, splinting, ergonomic job analysis, hand therapy. The increased costs from nonoperative treatment were due to longer care and longer time off work; these also increased the overall cost of treatment. < Lyall JM, Gliner J, Hubbell MK: Treatment of worker’s compensation cases of carpal tunnel syndrome: an outcome study. J Hand Ther 15:251-9, 2002.> A longer duration of symptoms, i.e. a delay to definitive surgical treatment, has also been associated with a longer time to return to work, implying that earlier definitive surgical treatment reduces the amount of time off of work. < Nancollas MP, Peimer CA, Wheeler DR, Sherwin FS: Long-term results of carpal tunnel release. J Hand Surg [Br] 20:470-4, 1995.> Shin also found carpal tunnel release to be superior to nonoperative management, with decreased disability, and a decreased necessity for job modifications and restrictions compared to those who did not undergo surgical release. < Shin AY, Perlman M, Shin PA, Garay AA: Disability outcomes in a worker’s compensation population: surgical versus nonsurgical treatment of carpal tunnel syndrome. Am J Orthop 29:179-84, 2000.>
Immobilizing braces
A rigid splint can keep the wrist straight.
The importance of wrist braces and splints in the carpal tunnel syndrome therapy is known, but many people are unwilling to use braces. In 1993, The American Academy of Neurology recommend a non-invasive treatment for the CTS at the beginning (except for sensitive or motor deficit or grave report at EMG/ENG): a therapy using splints was indicated for light and moderate pathology.[59] Current recommendations generally don’t suggest immobilizing braces, but instead activity modification and non-steroidal anti-inflammatory drugs as initial therapy, followed by more aggressive options or specialist referral if symptoms do not improve.[60][61]
Many health professionals suggest that, for best results, one should wear braces at night and, if possible, during the activity primarily causing stress on the wrists.[62][63]
Localized corticosteroid injections
Corticosteroid injections can be quite effective for temporary relief from symptoms of CTS for a short time-frame while a patient develops a longterm strategy that fits with his/her lifestyle.[64] In certain patients, an injection may also be of diagnostic value. This treatment is not appropriate for extended periods, however. In general, medical professionals prescribe local steroid injections only until other treatment options can be identified. For most patients, surgery is the only option that will provide permanent relief.[65]
Other medication
A more aggressive pharmaceutical option is an injection of cortisone, to reduce swelling and nerve pressure within the carpal tunnel. The role of Methylcobalamin (vitamin B12) in CTS is debatable and uncertain. [66]
Carpal tunnel release surgery
Scars from carpal tunnel release surgery. Two different techniques were used. The left scar is 6 weeks old, the right scar is 2 weeks old. Also note the muscular atrophy of the thenar eminence in the left hand, a common sign of advanced CTS
Carpal Tunnel Syndrome Operation
Release of the transverse carpal ligament is known as “carpal tunnel release” surgery. It is recommended when there is static (constant, not just intermittent) numbness, muscle weakness, or atrophy, and when night-splinting no longer controls intermittent symptoms.[67] In general, milder cases can be controlled for months to years, but severe cases are unrelenting symptomatically and are likely to result in surgical treatment.[68]
Procedure
In carpal tunnel release surgery, the goal is to divide the transverse carpal ligament in two. This is a wide ligament that runs across the hand, from the scaphoid bone to the hamate bone and pisiform. It forms the roof of the carpal tunnel, and when the surgeon cuts across it (i.e., in a line with the ring finger) it no longer presses down on the nerve inside, relieving the pressure.[69]
There are several carpal tunnel release surgery variations: Each surgeon has differences of preference based on his or her personal beliefs and experience. All techniques have several things in common, involving brief outpatient procedures, palm or wrist incision(s), and cutting of the transverse carpal ligament.[citation needed]
The two major types of surgery are open carpal tunnel release and endoscopic carpal tunnel release. Most surgeons historically have performed the open procedure, widely considered to be the gold standard. However, since the 1990s, a growing number of surgeons now offer endoscopic carpal tunnel release.[citation needed]
Open surgery involves an incision on the palm about an inch or two in length. Through this incision, the skin and subcutaneous tissue is divided, followed by the palmar fascia, and ultimately the transverse carpal ligament.[citation needed]
Endoscopic carpal tunnel release
Endoscopic techniques or endoscopic carpal tunnel release involve one or two smaller incisions (less than half inch each) through which instrumentation is introduced including a synovial elevator, probes, knives, and an endoscope used to visualize the underside of the transverse carpal ligament.[70] The endoscopic methods do not divide the subcutaneous tissues or the palmar fascia to the same degree as the open method does.[71] Many studies have been done to determine whether perceived benefits of a limited endoscopic or arthroscopic release are significant. Brown et al. conducted a prospective, randomized, multi-center study and found no significant differences between the two groups with regard to secondary quantitative outcome measurements.[72] However, the open technique resulted in more tenderness of the scar than the endoscopic method. A prospective randomized study done in 2002 by Trumble revealed that good clinical outcomes and patient satisfaction are achieved more quickly with the endoscopic method. Single-portal endoscopic surgery is a safe and effective method of treating carpal tunnel syndrome. There was no significant difference in the rate of complications or the cost of surgery between the two groups. However, the open technique caused greater scar tenderness during the first three months after surgery, and a longer time before the patients could return to work.[73] In addition, in patients without workers compensation issues, the single-incision endoscopic carpal tunnel release led to less palmar tenderness and a quicker return to work compared to the two-incision endoscopic carpal tunnel release (Palmer DH, Paulson JC, Lane-Larsen CL, Peulen VK, Olson JD: Endoscopic carpal tunnel release: a comparison of two techniques with open release. Arthroscopy 9:498-508, 1993.)
Many surgeons have embraced limited incision methods. It is considered to be the procedure of choice for many of these surgeons with respect to idiopathic carpal tunnel syndrome. Supporting this are the results of some of the previously mentioned series that cite no difference in the rate of complications for either method of surgery. Thus, there has been broad support for either surgical procedure using a variety of devices or incisions. The primary goal of any carpal tunnel release surgery is to divide the transverse carpal ligament and the distal aspect of the volar ante brachial fascia, thereby decompressing the median nerve.[74] Despite these views, some surgeons have suggested that in their own hands endoscopic carpal tunnel release has been associated with a higher incidence of median nerve injury, and for this reason it has been abandoned at several centers in the United States. At the 2007 meeting of the American Society for Surgery of the Hand, a former advocate of endoscopic carpal tunnel release, Thomas J. Fischer, MD, retracted his advocacy of the technique, based on his own personal assessment that the benefit of the procedure (slightly faster recovery) did not outweigh the risk of injury to the median nerve. Contrary to this one or any one opinion of any individual surgeon it has been shown that while there is a learning curve for a hand surgeon who begins to use an endoscopic technique to release the transverse carpal ligament no significant safety issues or morbididty associated with the endoscopic method exist.[75] The use of endoscopic carpal tunnel release has continued to spread around the world and clinical and nerve electrophysiological states are significantly improved at the long-term follow-up after endoscopic carpal tunnel release.[76] A meta-analysis supports the conclusion that endoscopic carpal tunnel release is favored over the open carpal tunnel release in terms of a reduction in scar tenderness and increase in grip and pinch strength at a 12-week follow-up [77]
Experimental procedures
Balloon carpal tunnelplasty is an experimental technique that uses a minimally invasive balloon catheter director to access the carpal tunnel. As with a traditional tissue elevator/expander, balloon carpal tunnelplasty elevates the carpal ligament, increasing the space in the carpal tunnel. As an experiment it has been described but there are no peer reviewed series available in the current hand surgical literature that review or comment upon the procedure. The technique is performed through a one-centimeter incision at the distal wrist crease. It is monitored and expansion is confirmed by direct or endoscopic visualization. The technique’s secondary goals are to avoid to incision in the palm of the hand, to avoid cutting of the transverse carpal ligament, and to maintain the biomechanics of the hand.[78]
Efficacy
Surgery to correct carpal tunnel syndrome has a high success rate. Up to 90% of patients were able to return to their same jobs after surgery.[79][80][81] In general, endoscopic techniques are as effective as traditional open carpal surgeries,[82][83] though the faster recovery time typically noted in endoscopic procedures is felt by some to possibly be offset by higher complication rates.[84][85] Success is greatest in patients with the most typical symptoms. The most common cause of failure is incorrect diagnosis, and it should be noted that this surgery will only mitigate carpal tunnel syndrome, and will not relieve symptoms with alternative causes. Recurrence is rare, and apparent recurrence usually results from a misdiagnosis of another problem.[citation needed] Complications can occur, but serious ones are infrequent to rare.[citation needed]
Carpal tunnel surgery is usually performed by a hand surgeon, orthopaedic surgeon, or plastic surgeon. Some neurosurgeons and general surgeons also perform the procedure.[citation needed]
Ultrasound physiotherapy treatment
Some claim that ultrasound to the wrist gives significant improvement of symptoms in people with CTS.[86] A treatment process may consist of 20 sessions of 15 minutes of ultrasound applied to the area over the carpal tunnel at a frequency of 1 MHz, and a power of 1.0 W/cm2.[86]
However, many studies have shown no effect.[87][88] Given these inconsistencies, the role of ultrasound in the treatment of CTS is debatable and it should be considered an experimental treatment.
Physiotherapy/Occupational Therapy
One review of the evidence for possible symptom reduction found good evidence (level B recommendations) for splinting, ultrasound, Laser, Tens, nerve gliding exercises/Neural mobilization, carpal bone mobilization, magnetic therapy, and yoga for people with carpal tunnel syndrome.[89] However, a recent evidence based guideline produced by the American Academy of Orthopedic Surgeons assigned lower grades to most of these treatments.[90]
Again, some claim that pro-active ways to reduce stress on the wrists, which alleviates wrist pain and strain, involve adopting a more ergonomic work and life environment. For example, some have claimed that switching from a QWERTY computer keyboard layout to a more optimised ergonomic layout such as Dvorak was commonly cited as beneficial in early CTS studies, however some meta-analyses of these studies claim that the evidence that they present is limited.[91][92]
Prognosis
Most people relieved of their carpal tunnel symptoms with conservative or surgical management find minimal residual or “nerve damage”.[93] Long-term chronic carpal tunnel syndrome (typically seen in the elderly) can result in permanent “nerve damage”, i.e. irreversible numbness, muscle wasting, and weakness.
While outcomes are generally good, certain factors can contribute to poorer results that have little to do with nerves, anatomy, or surgery type. One study showed that mental status parameters or alcohol use yields much poorer overall results of treatment.[94]
Recurrence of carpal tunnel syndrome after successful surgery is rare.[95] If a person has hand pain after surgery, it is most likely not caused by carpal tunnel syndrome. It may be the case that the illness of a person with hand pain after carpal tunnel release was diagnosed incorrectly, such that the carpal tunnel release has had no positive effect upon the patient’s symptoms.[citation needed]
Epidemiology
Carpal tunnel syndrome can affect anyone. In the U.S., roughly 1 out of 20 people will suffer from the effects of carpal tunnel syndrome. Caucasians have the highest risk of CTS compared with other races such as non-white South Africans.[96] Women suffer more from CTS than men with a ratio of 3:1 between the ages of 45–60 years. Only 10% of reported cases of CTS are younger than 30 years.[96] Increasing age is a risk factor. CTS is also common in pregnancy.
History
The condition known as carpal tunnel syndrome had major appearances throughout the years but it was most commonly heard of in the years following World War II.[97] Individuals who had suffered from this condition have been depicted in surgical literature for the mid-19th century.[97] In 1854, Sir James Paget was the first to report median nerve compression at the wrist in a distal radius fracture.[98] Following the early 20th century there were various cases of median nerve compression underneath the transverse carpal ligament.[98] Carpal Tunnel Syndrome was most commonly noted in medical literature in the early 20th century but the first use of the term was noted 1939. Physician Dr. George S. Phalen of the Cleveland Clinic identified the pathology after working with a group of patients in the 1950s and 1960s.
Notable cases
- HRH Prince Philip, husband of Queen Elizabeth II[99]
- Mike Dirnt, bassist with the band Green Day[100]
- Michael Einziger, guitarist with the band Incubus
- Kelly Shaefer, guitarist and singer with the band Atheist